Schreiber Lab
Molecular Mechanisms in Autoimmune Kidney Disease
Profile
ANCAs are IgG autoantibodies that target antigens present in the cytoplasm of neutrophils and monocytes. Once activated, those myeloid cells adhere to and damage the endothelium, leading to vascular inflammation and necrosis. Lymphoid cells including T und T helper cells have also been described to be involved in the development of AAV.
Our group aims to better understand the complex interaction between innate and adaptive immunity in AAV, to characterize the cellular and molecular pathways involved and to identify targets for novel treatment strategies.
Team
Group leader
PD Dr. Adrian Schreiber
adrian.schreiber@charite.de
+49(30)450540-293
Scientists
Dr. Anthony Rousselle
anthony.rousselle@charite.de
anthony.rousselle@mdc-berlin.de
+49(30)450540-284
Dr. Marlene Weiß
marlene.weiss@charite.de
Dr. Dörte Lodka
doerte.lodka@charite.de
+49(30)450540-293
Janis Sonnenmann
janis.sonnemann@charite.de
Technical Assistants
Sylvia Lucke
sylvia.lucke@charite.de
sylvia.lucke@mdc-berlin.de
+49(30)450540-293
Tanja Filipowski
tanja.filipowski@charite.de
+49(30)450540-293
Research
- Role of monocytes in ANCA-associated vasculitis (AAV)
The interaction of ANCA IgG with neutrophils has been established as a causative mechanism in inducing systemic vasculitis and organ damages. In contrast, any role of monocytes remain poorly described. Using CCR2-DTR mice, we showed that depletion of CCR2+ Ly6Chi inflammatory monocytes (and monocyte-derived cells) with diphtheria toxin significantly reduced crescent formation, glomerular necrosis and renal leukocyte infiltration in an AAV murine model.
Our findings establish an important role of monocytes in the development of AAV. CCR2+ Ly6Chi inflammatory monocytes serve as precursors for macrophages, dendritic cells and CCR2-Ly6Clo patrolling monocytes. Because all these cells were depleted in CCR2-DTR mice treated with diphtheria, the exact contribution of each monocyte subset requires further experiments. In addition, an atypical monocyte subset (Ly6Clo Msr1+Caecam1+) important for the development of fibrosis has been described. We are currently working with different knock out mice and depletion strategies to better describe the role of the different monocyte subsets in AAV.
- Interplay between Th17 T cells and ANCA-stimulated neutrophils
The regulation of T cells immunity by neutrophils remains unknown in AAV. NGAL (neutrophil gelatinase-associated lipocalin; also called lipocalin 2) belongs to the lipocalin superfamily and is found in neutrophil granules. NGAL is currently used as a marker of human kidney disease.
We found that ANCA-stimulated neutrophils degranulate a huge amount of NGAL. These results suggest a potential role of neutrophil NGAL in AAV. Intriguingly, we found that mice with either a total or a hematopoietic specific NGAL deletion developed an exacerbated NCGN with an increased renal Th17 cell infiltration compared to WT mice. IL17A knockout mice and NGAL/Il17A double knockout mice were protected from systemic vasculitis proving that Th17 cells indeed play a central role in AAV and confirming a link between NGAL and Th17 immunity. We are currently investigating the exact mechanism(s) by which neutrophil NGAL modulate Th17 T cell proliferation/differentiation/infiltration.
- Molecular regulation of ANCA-induced neutrophil extracellular traps (NETs)
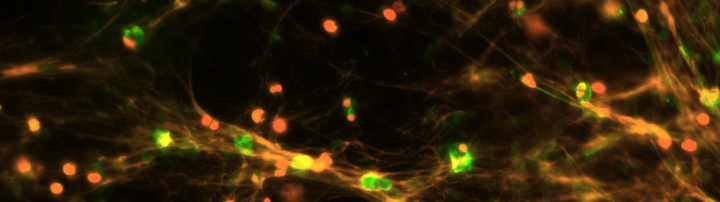
ANCA-dependent neutrophil activation induces a multitude of cellular events including the generation of NETs. NETS are lattice-like structures containing DNA, histone and neutrophil granule proteins including both most common ANCA antigens MPO and PR3. NETs are thought to play a major role in AAV but their exact roles and regulation remain to be described.
We recently put in evidence that NETs generation is regulated by the activation of a programmed form of cell death (necroptosis) via receptor-interacting protein kinase 1 and 3 (RIPK1/3) and the mixed lineage kinase domain-like protein (MLKL). We further showed that NETs generated by ANCA-stimulated neutrophils caused direct damage to endothelial cells in vitro. This effect was prevented by I) pharmacological inhibition of necroptosis, II) enzymatic NETs degradation and III) genetic deletion of RIPK3. In vivo, mice with a genetic deletion of RIPK3 or MLKL were protected from the development of AAV.
We could also demonstrate that NETs provided a scaffold for the activation of alternative complement, which in turn further contributed to the endothelial cell damage in vitro. Altogether, we identified a mechanistic link between ANCA-activated neutrophils, NETs, necroptosis, the alternative complement and endothelial damage. We are currently looking for additional pathways and mechanisms, which might be involved in the regulation and formation of NETs.

