Unlocking skin cells' role in pain and touch
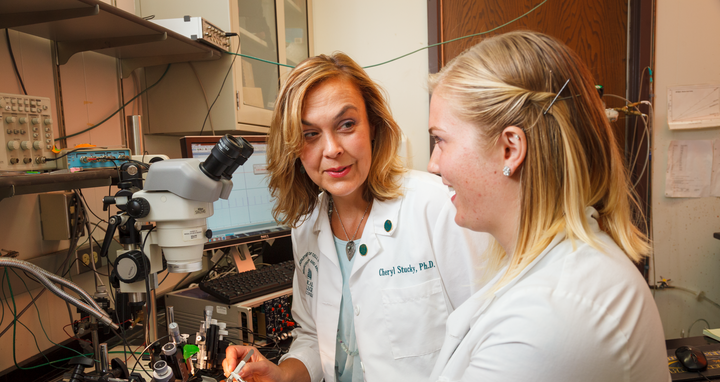
Pain has always been a focus in Professor Gary Lewin’s lab. Cheryl L. Stucky was the first postdoctoral researcher in Lewin’s lab, working there from 1997 to 1999. It turned out to be a launching pad. She went right from Gary Lewin’s lab to starting her own research group at the Medical College of Wisconsin. Professor Cheryl L. Stucky has since worked in neuroscience for over 25 years and has published over 116 original research articles. Now, she is a senior scientist with an endowed research chair and serves as Director of the Pain Division at the Neuroscience Research Center.
Her research focuses on somatosensory and pain mechanisms. In particular, Stucky investigates how ion channels on pain-sensitive neurons contribute to the sensations of pain and touch, for example in chemotherapy-induced neuropathic pain. On November 8, she will visit the Max Delbrück Center and give a talk as part of our “Pathway series”. Her topic: “Beyond the Barrier: Skin cells participate in touch and pain”. In our interview with Cheryl Stucky, she reflects on how her time at the Max Delbrück Center has shaped her career path and shares what she is working on today.
What is the first thing that comes to mind when you think of your time at the Max Delbrück Center?
Professor Cheryl L. Stucky: I really enjoyed the collaborative spirit at the Max Delbrück Center, along with the high-caliber science. At the time, I was not at all familiar with the patch-clamp technique, which can be used to visualize the current through individual ion channels in the membrane of a cell. I learned from several wonderful and generous postdoc fellows in Helmut Kettenmann’s lab. Gary Lewin was my PI, and I appreciated how clever and creative he was then — and has been all his career. His avant-garde approach makes Gary very fun to work with. He is also very driven, and I enjoyed his competitive spirit and that he is a really outstanding PI mentor.
What did you work on back then?
I used patch-clamp techniques to study the functional properties of pain receptors (nociceptors). Gary Lewin and I discovered that a class of non-peptide expressing nociceptors had distinct physiological properties. We also worked on how neurotrophins modulate the development, survival and function of nociceptors. And we began exploring the ion channels that underlie mechanical sensitivity in sensory neurons.
“In Berlin, I have found my niche”
How did this time shape your career path?
My work with Gary gave me the insight and preliminary data to apply for my first NIH grant, which was funded on first submission. The electrophysiological recording methods I learned in Gary’s lab — both patch-clamp recordings and skin nerve teased-fiber recordings — are key approaches that I have used in my lab for the last 23 years and continue to teach my students and postdocs. These methods remain state-of-the-art and informative for uncovering sensory transduction and pain mechanisms in the somatosensory field today. I’m extremely grateful that I learned these approaches because they gave me a unique niche and a path of my own to follow for my career. Working with Gary showed me how to ask unique and clever research questions and also bridge basic to clinical research using novel approaches.
What are you focusing on today?
In my laboratory, we deal with five different types of pain. First, there is chemotherapy-induced neuropathic pain. Recently, we discovered that a protein in skin cells called Piezo1 controls touch sensitivity in normal skin. Our new, unpublished data suggest that this protein also controls the debilitating touch pain caused by chemotherapy treatment.
Our second area of research is pain due to nerve damage that can occur after an accident or surgical procedures. We want to identify the cell types that contribute to nerve damage and understand how these cells signal to cause persistent pain long after the injuries have healed.
Another very important topic is pain from sickle cell disease. Sickle cell pain is devastating, still vastly understudied and lacks effective treatment options. Our lab is one of the few laboratories worldwide that deals with this issue. We also study pain in Fabry disease, an inherited neurological disorder caused by a deficiency of enzymes. Affected individuals suffer from episodic and chronic pain throughout their lives.
Last but not least, we are investigating TRPC5 (transient receptor potential canonical 5) as a new target for drugs against persistent inflammatory pain. TRPC5 is a protein found on many different cell types. Human neurons also express TRPC5. In several rodent models, we found that the protein is involved in the control of tactile and spontaneous pain. In this respect, TRPC5 inhibitors could possibly be an agent against that pain.
An exciting development for all projects is that we are garnering human skin, plasma and neural tissues to better translate our results in rodents to humans, in order to validate pain mechanisms in patients.
The interview was conducted by Jana Ehrhardt-Joswig.