Key processes in acute kidney injury revealed
Joint press release of the Max Delbrück Center and Charité – Universitätsmedizin Berlin
The kidneys are among the most important organs in the human body. They filter waste products from the blood, control body fluid composition and blood pressure, influence energy metabolism, and produce vital hormones. If kidney function is impaired – as is the case in acute kidney injury – there can be severe consequences. “Acute kidney injury is a frequent and serious complication in critically ill patients, affecting about half of our intensive care unit patients,” says Dr. Jan Klocke of Charité’s Department of Nephrology and Medical Intensive Care. “The condition is often underestimated, despite the fact that acute kidney injury is associated with increased mortality and patients can suffer permanent damage, even complete loss of kidney function.”
We try to stabilize affected patients, but so far it is usually not possible to reverse the destructive processes in the kidney with targeted treatments.
Acute kidney injury can accompany a wide range of diseases. It often occurs in conjunction with cardiovascular diseases or severe infectious diseases such as COVID-19, but also after surgical interventions or in association with drug treatment. There are often no concrete treatment options. “We try to stabilize affected patients, but so far it is usually not possible to reverse the destructive processes in the kidney with targeted treatments,” says Dr. Christian Hinze, who played a key role in supervising one of the studies at Charité and in the Lab of Professor Kai-Schmidt-Ott at the Max Delbrück Center. Now, Schmitt-Ott is director at the clinic for nephrology at Hannover Medical School (MHH), where Hinze now works as well. “Up to now, little has been known about which mechanisms are at play in the kidney cells. The aim of our studies was to shed some light on this, with the long-term goal of improving the treatment provided to our patients in the clinic,” says Hinze. The studies were conducted in close collaboration between Charité – Universitätsmedizin Berlin; the Berlin Institute for Medical Systems Biology of the Max Delbrück Center (MDC-BIMSB); the German Rheumatism Research Center Berlin (DRFZ), a Leibniz Institute; and the Hannover Medical School.
Zooming into the cell
Acute kidney injury is often triggered by an insufficient supply of blood to the kidneys, causing the cells there to no longer receive sufficient oxygen and nutrients – and to react with stress. The cells go into a kind of alarm mode and produce signal substances that can lead to inflammatory and remodeling processes (fibrosis) in the surrounding tissue. It is known from animal model studies that epithelial cells – the cells that line the fine renal tubules – are involved in these inflammatory and fibrotic processes. This was demonstrated using a novel state-of the-art method called single-cell sequencing, which enables researchers to create a detailed profile of the molecular gene expression profiles of thousands of individual cells. But what happens on the cellular level when humans suffer from acute kidney injury?
This is the question that research teams led by Dr. Hinze and Dr. Klocke set out to investigate. The two recently published studies are among the first to ever investigate the molecular processes in AKI using single-cell technologies in human kidney cells. Cooperating with the Lab of Professor Nikolaus Rajewsky at MDC-BIMSB, the scientists examined cells taken from tissue and urine samples of more than 40 patients and analyzed the molecular patterns of more than 140,000 cells using state-of-the-art bioinformatics approaches. “Single-cell sequencing allows us to virtually zoom into each cell and see which genes are active in that cell at that point in time,” explains Hinze. “From this, we can determine whether that particular kidney cell is currently functioning normally, is under stress, or is about to die. This cutting-edge technology gives us an understanding of acute kidney injury in unprecedented detail.”
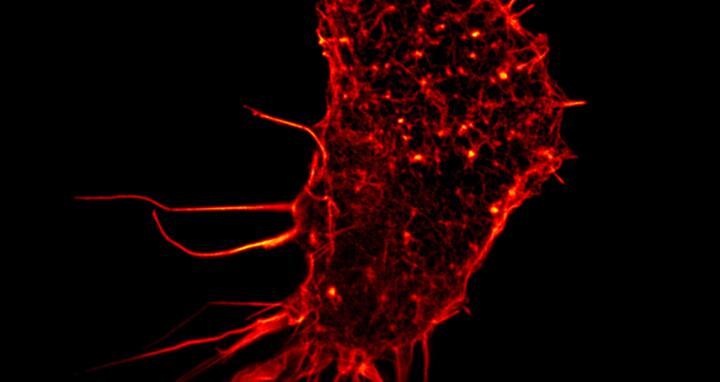
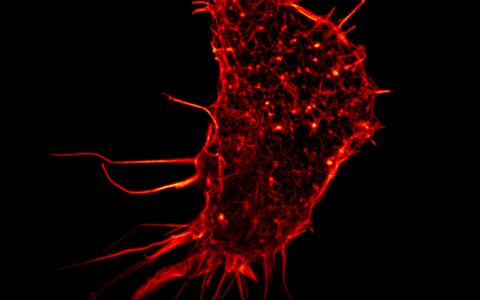
Microscopic image of a single renal cell.
The team was also able to show that different cell types of the kidney react quite differently to acute kidney injury, with the strongest response observed in the epithelial cells of the renal tubules. These are the smallest functional units of the kidney and consist of several segments. It was known from animal models that epithelial cells of a specific early renal tubule segment were mainly affected by acute kidney injury. However, the results of the latest studies on human kidney cells have revealed that the epithelial cells of almost all tubule segments are involved in the injury processes. “This illustrates once again how important it is that we study human systems and learn to understand them better,” says Hinze. “In the different types of epithelial cells, we were able to identify certain molecular patterns that occurred in all patients with acute kidney injury, but at individual abundances. In the future, these findings could help doctors to better assess the risk for severe disease progression.”
A promising start for diagnostics
In clinical practice, physicians ideally need a fast, non-invasive, and precise testing method to clearly diagnose acute kidney injury at an early stage. In order to get closer to this vision for the future, Klocke started searching for epithelial cells in urine samples. Hardly any cells are found in the urine of healthy people. But in those with acute kidney injury, epithelial cells detach from the renal tubule and are excreted into the urine. However, since cells do not survive in urine for long, there were initial doubts as to whether the cells would still be intact and whether their molecular state could even be measured using single-cell sequencing. “We processed the urine samples within four to six hours, and it actually worked very well,” says Klocke. The researchers were able to determine from which segment of the renal tubules the cells came from and which genetic programs they had activated in response to kidney damage. “The information provided by the cells from the urine samples matched that of the corresponding cells from tissue samples,” says Klocke. “Thus, urine provides us with an uncomplicated and patient-friendly method of obtaining sample material for further investigations – in order to identify biomarkers and, in the long term, perhaps reduce or even replace kidney biopsies.”
With the two current studies, the research teams have provided completely new insights into the cellular mechanisms in acute kidney injury using single cell sequencing as well as promising approaches for future diagnostic procedures and personalized therapies. In further studies, they plan to enroll a larger number of patients, investigate the cellular responses in different underlying diseases, and uncover other fundamental molecular mechanisms of acute kidney injury using cell cultures.
Further information
- Department of Nephrology and Medical Intensive Care
- CRC 1365 “Renoprotection” hosted by Charité
- Berlin Institute for Medical Systems Biology (BIMSB)
- Video interview with Christian Hinze about his research at the Max Delbrück Center (available only in German)
Literature
Christian Hinze et al. (2022): “Single-cell transcriptomics reveals common epithelial response patterns in human acute kidney injury”; Genome Med. DOI: s13073-022-01108-9
Jan Klocke et al. (2022): “Urinary single-cell sequencing captures intrarenal injury and repair processes in human acute kidney injury”; Kidney Int. DOI: 10.1016/j.kint.2022.07.032
Contacts
Dr. Jan Klocke
Department of Nephrology and Medical Intensive Care
Charité – Universitätsmedizin Berlin
t:+49 30 450 614 62
jan.klocke@charite.de
Prof. Dr. Nikolaus Rajewsky
Director of the Berlin Institute for Medical Systems Biology at the Max Delbrück Center (MDC-BIMSB)
+49 (0)30 9406-2999 (office)
rajewsky@mdc-berlin.de
Christina Anders
Editor, Communications Department
Max Delbrück Center
Tel.: +49 30 9406-2118
christina.anders@mdc-berlin.de or presse@mdc-berlin.de
Downloads
Microscopic image of a single renal cell. Credit: Human kidney cell, Gated-STED microscopy.Alison Dun, ESRIC (Edinburgh Super-Resolution Imaging Consortium). Attribution 4.0 International (CC BY 4.0)
- Max Delbrück Center
-
-
The Max Delbrück Center for Molecular Medicine in the Helmholtz Association (Max Delbrück Center) is one of the world’s leading biomedical research institutions. Max Delbrück, a Berlin native, was a Nobel laureate and one of the founders of molecular biology. At the locations in Berlin-Buch and Mitte, researchers from some 70 countries study human biology – investigating the foundations of life from its most elementary building blocks to systems-wide mechanisms. By understanding what regulates or disrupts the dynamic equilibrium of a cell, an organ, or the entire body, we can prevent diseases, diagnose them earlier, and stop their progression with tailored therapies. Patients should benefit as soon as possible from basic research discoveries. The Max Delbrück Center therefore supports spin-off creation and participates in collaborative networks. It works in close partnership with Charité – Universitätsmedizin Berlin in the jointly run Experimental and Clinical Research Center (ECRC), the Berlin Institute of Health (BIH) at Charité, and the German Center for Cardiovascular Research (DZHK). Founded in 1992, the Max Delbrück Center today employs 1,800 people and is funded 90 percent by the German federal government and 10 percent by the State of Berlin.
- Charité – Universitätsmedizin Berlin
-
-
With a total of 3,001 beds, Charité – Universitätsmedizin Berlin is one of the largest university hospitals in Europe. Charité spans 4 campuses and comprises approximately 100 Departments and Institutes. In 2015, Charité treated more than 142,000 outpatient and more than 663,000 inpatient cases. With approximately 16,900 staff employed across the Charité group of companies, Charité is one of the largest employers in Berlin. In 2015, the Charité university hospital recorded a turnover of more than €1.6 billion. The areas of research, teaching, and health care delivery are intricately linked, resulting in a working relationship that is characterized by interdisciplinary cooperation. In 2015, Charité was able to secure more than €149 million in third-party funding, as well as approximately €202 million in state funding for research and teaching. With approximately 7,000 future physicians and dentists currently enrolled in degree courses, Charité is one of the largest medical faculties in Germany.
- Collaborative Research Center “Renoprotection”
-
-
The two studies were conducted in the context of the Collaborative Research Center (CRC) 1365 “Renoprotection,” which is funded by the German Research Foundation. The interdisciplinary research consortium aims to better understand the overarching injury mechanisms involved in acute kidney injury and chronic kidney disease, as well as to identify potential therapeutic targets.